Digestive system
In previous blogs we’ve talked about the different nutrients our body needs. We have yet to discuss the way our body absorbs and processes these substances. And to do so, we’re visiting the digestive system today. So how does your food travel from mouth to bottoms?
Organs
In order to better understand the digestive system, we’ll be examining the organs involved.
The mouth
Digestion starts at the top, in your mouth. A signal is sent to your brain whenever you see, smell or taste food. This activates neurons in your brain: the parasympathetic nervous system. This is step one of digestion.
Saliva makes food wet to be able to swallow it, but also coats it in protective matter: antibodies to kill any pathogen. It also contains amylose, an enzyme that splits starch in to smaller molecules.
Besides chemical digestion, due to enzymes in saliva, we also speak of mechanical digestion. By chewing with your teeth and moving your tongue, bites get smaller and compacted to a ball. The tongue pushes the ball backwards which initiates the swallow reflex. This temporarily closes of the nasal cavity and trachea so the food can enter the esophagus.
The oesophagus
The esophagus carries food over from the throat to the stomach. It is about 25cm long and the width varies from 1.5 to 2 cm. The esophagus lies behind the trachea and the heart, and sits in front of the vertebral column. It travels through the diafragma before it enters the stomach. The food is slowly pushed through using a peristaltic movement. The esophagus makes use of both smooth muscles and skeletal muscles to extend and retract itself.
The inside is covered in a thick layer of slime to make food travel down easily. We call this layer: mucosa. The esophagus does not break down any nutrients during its process.
The stomach
Food reaches your stomach coming from the oesophagus. It gets mixed with gastric juice to break down the food particles, making them more soluble. The most important functions of the stomach are the initiation of carbohydrate and protein digestion, as well as turning the food and juice combination in to chyme.
The stomach is located in de upper left part of your belly, directly below the diaphragm. In front of the stomach is the liver, behind that is the pancreas, the kidneys, the spleen and the large intestine.
The cardia is the opening between the oesophagus and the stomach. The upper part of the stomach is called the fundus. The fundus adjusts to the variable quantities of food taken in by relaxing its muscular walls. The middle part (and also biggest part) of the stomach is called the gastric body, it mainly serves as storage for foods and fluids. The antrum, the bottom part of the stomach, is funnel-shaped. The broad end connects to the lower part of the stomach body and the narrow end connects to the pyloric canal, which flows into the duodenum (the upper part of the small intestine). The pyloric canal, the smallest part of the stomach, is the exhaust of the stomach to the duodenum. It has a diameter of about 2 cm. wide.
The stomach can widen itself in order to take in about a liter of food or fluids, without expanding its pressure. The expansion of the gastric body by food activates a reflex that initiates muscle activity in the antrum.
The stomach moves and kneads the food in different ways. This ensures that digestion can take place easily, and it helps to distribute and mix the food well before it moves to the duodenum.
The inner surface of the stomach is lined with a mucous membrane called the gastric mucosa. The mucosa is always covered with a layer of thick mucus secreted by tall columnar epithelial cells. Stomach mucus has two main purposes; it provides a smooth layer to facilitate the movement of food and it forms a protective layer over the mucous membrane epithelium of the stomach cavity. The stomach acid has a low pH that could affect the inside of the stomach. This mucous layer protects the stomach from the low pH of the stomach acid.
The mucosa, or inner mucous membrane of the stomach consists of gastric pits that later (deeper down in the mucous membrane) transform into gastric glands. The glands contain cells that secrete substances to aid the digestion of food.
Mucosal cells
The mucus cells are cells that separate the slimes for the inside of the stomach. This creates a protective layer against stomach acids. It also excretes bicarbonate (HCO3-). This substance neutralises the pH of the stomach acid so that no damage can be done to the cells (Figure 1).
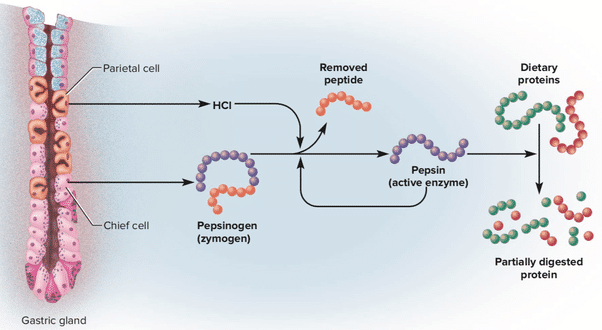
Figure 1.
Chief Cells
These cells excrete pepsinogen, pepsinogen still has to be converted to the active pepsin, which is done by HCL. Pepsin is a protease (protein-digesting enzyme), so when this conversion from pepsinogen to pepsin has taken place, protein digestion can commence in the stomach.
G-cells
These endocrine cells secrete the acid-stimulating hormone gastrin in response to a decreased acidity of the stomach contents when food enters the stomach and the stomach expands. Gastrin then enters the bloodstream and is transported in the circulation to the mucosa in the middle part of the stomach, where it binds to receptors on the outer membrane of the parietal cells. The formed gastrin receptor complex stimulates the secretion of HCL.
Parietal cells
Parietal cells secrete hydrogen ions that combine with the chloride ions to form hydrochloric acid (HCL) as shown in Figure 2. The produced acids then get transported to the lumen of the gland, which then proceeds to to the stomach. This process only takes place when one or more types of receptors on the outer membrane of the parietal cell are offered to histamine, gastrin or acetylcholine. Prostaglandins, hormone-like substances present in almost all tissues and body fluids, inhibit the secretion of hydrochloric acid.
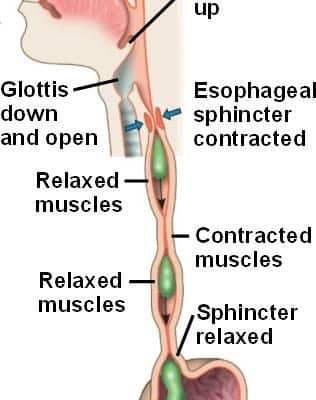
Figure 2.
The speed with which the stomach is emptied depends on the physical and chemical composition of the meal. Liquids drain faster than solids. The peristaltic movement in the stomach helps to transfer the chyme from the stomach to the small intestine. In a normal situation, food remains in the stomach for 2 to 6 hours, after which it is released to the small intestine in portions via the sphincter (shutter muscle).
The small intestine
The small intestine is the main organ of the digestive tract. The primary functions of the small intestine are mixing and transporting contents, producing enzymes and other components essential for digestion and nutrient absorption. Most of the processes that dissolve and reduce carbohydrates, proteins and fats to relatively simple organic compounds take place in the small intestine.
The small intestine, 670 to 760 cm long and 3 to 4 cm in diameter, is the longest part of the digestive tract. It begins at the pylorus, the junction with the stomach, and ends at the ileocaecal valve, the junction with the large intestine. The main functional segments of the small intestine are the duodenum, jejunum and ileum.
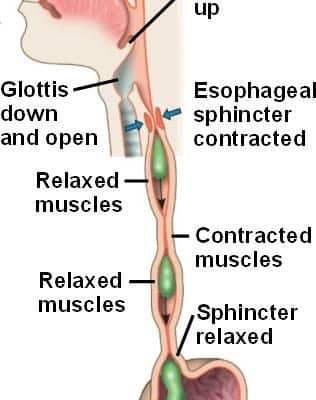
Figure 3.
Although the small intestine is only 3 to 4 cm in diameter and about 7 metres long, it is estimated that the total absorption area is about 4500 square metres. This is possible because of the small protrusions present on the inside of the intestine. These protrusions are called vili. The notches between the vili are called crypts. These are mainly the cells that secrete fluid and hormones. The stem cells that ensure constant renewal of the intestinal cells are also present there.
The large intestine
The large intestine, or colon, serves as a reservoir for fluids coming from the small intestine. It has a much larger diameter than the small intestine, about 2.5 cm as opposed to 6 cm, with 150 cm in length it is also less than a quarter the length of the small intestine. The primary functions of the large intestine are to absorb water; to maintain the osmolarity of the level of dissolved substances of the blood by separating and absorbing electrolytes (substances such as sodium and chloride, which are in solution and take on electric charge) from the chyme; and to store faeces until it can be excreted.
The pancreas
The pancreas is a long, narrow gland that lies across the upper abdomen, behind the stomach and spleen. The pancreas is both an exocrine and endocrine gland. The exocrine tissue, called acinar tissue, produces important enzymes that are transferred to the small intestine for digestion. The endocrine tissue (islets of Langerhans) produces two hormones (insulin and glucagon) that are important in regulating carbohydrate metabolism.
Acrine cells
The acinar cells fill more than 95% of the exocrine part of the pancreas. They produce a variety of digestive proteins, or enzymes that are mainly involved in the breakdown of food proteins (proteins), fats (lipids) and carbohydrates (amylases) in the gut. In the acinar cells, almost all enzymatic proteins are synthesised on ribosomes from amino acids transported by the bloodstream to the pancreas.
Islet cells
There are three types of islet cells, designated alpha, beta and delta, which make up about 2% of the total pancreatic mass. Islet cells are approximately 20-35% alpha, 60-75% beta and 5% delta. The alpha cells release glucagon, which leads to the breakdown of glycogen in the liver and an increase in the blood glucose level. Beta cells release insulin which actually does the opposite. Delta cells release somatostatin, whose effects inhibit the release of glucagon and insulin.
The liver
The liver is not only the largest gland in the body, but also the one with the most complex function. The main functions of the liver are to participate in the metabolism of proteins, carbohydrates and fat to synthesise cholesterol and bile acids. Synthesising bile acids is necessary for the production of bile to participate in the transport of bilirubin to stabilise and transport certain drugs and to regulate the transport and storage of carbohydrates.
Bile ducts
Bile is made by the liver and then stored in the gall bladder, when it is needed it is transported to the small intestine. Bile consists of salted cholesterol, bilirubin and foreign body waste.
Bile salts are made from steroids, bile acids and from amino acids. Bile salts make insoluble fats slightly more water-soluble, which is called emulsification. Most bile salts are reabsorbed at the end of the small intestine and returned to the liver via the portal vein.
Digestion of nutrients
We’ve established the journey our food has to take in order to be processed. Let’s see how these nutrients are absorbed by the body.
Digestion of carbohydrates
Carbohydrates are absorbed as monosaccharides (simple sugars such as glucose, fructose and galactose that cannot be further broken down by hydrolysis) or as disaccharides (carbohydrates such as sucrose, lactose, maltose and dextrin that can be hydrolysed into two monosaccharides). However, these simple molecules must be obtained by breaking down polysaccharides, complex carbohydrates containing many monosaccharides. The most important of these is amylose, a starch that accounts for 20% of carbohydrates in the diet. Amylose consists of a straight chain of glucose molecules bound to their neighbours by oxygen bonds. Most of the starch is amylopectin.
Only a small amount of starch is digested by salivary amylase, but even the amylase from the pancreas has little effect on the side chains of amylopectin and even less on the bonds in cellulose molecules. This explains the inability of humans to break down cellulose. There are several forms of amylase in pancreatic juice whose function is to hydrolyse complex carbohydrates into disaccharides and trisaccharide and amylopectin into dextrins. In the brush border and surface membrane of the epithelial enterocyte are the disaccharidase enzymes, lactase, maltase, sucrase and trehalose which hydrolyse maltose and dextrins to monosaccharides, glucose, galactose and fructose.
Glucose, one of the two monosaccharide components of table sugar (sucrose) and milk sugar (lactose), combines with phosphate in the liver cell and is either transported to peripheral tissues for metabolic purposes or stored as glycogen.
To absorb the carbohydrates, there are different ways of transport. The easiest way is passive transport: molecules move spontaneously into the blood. This does not require energy but generally involves a gradient difference. Passive transport occurs in the form of diffusion or osmosis.
In addition, many sugars are absorbed and moved via active transport. This is done with a carrier molecule or via transporters. Active transport always costs energy in the form of ATP, which is why molecules can also be transported in this way against the gradient, so that they do not always have to move from a high to a low concentration.
Active Transport can also be divided into two types: primary active transport, which is directly linked to the use of ATP and secondary active transport, which is indirectly linked to the use of ATP.
The absorption of carbohydrates in the small intestine involves secondary active transport, which means that ATP is needed but indirectly.
Two transporters are required for glucose uptake: the SGLT and the GLUT2 transporter. Glucose cannot be automatically taken up by the transporter, it needs a sodium gradient, the sodium gradient is caused by the sodium-potassium pump. The sodium gradient is caused by the sodium-potassium pump, which ensures that the sodium is transported out of the intestinal cell and that therefore less sodium remains in the intestines. The sodium-potassium pump works with ATP and is therefore an active transport.
As there is now less sodium present in the intestinal cells, the SGLT can transport sodium with the gradient, taking glucose with it as shown in Figure 4. Sodium is then pumped out again and glucose leaves the intestinal cell and is taken up into the capillary with the GLUT2 receptor.

Figure 4.
The digestion of fats
90% of the fats in food are triglycerides. Triglycerides are broken down by the enzymes lipase and colipase which are secreted in the pancreas and end up in the intestines. The triglycerides are broken down by the enzymes into monoglycerides and free fatty acids.
A property of fats is that they are not water-soluble. So in order to absorb fats, bile salts are needed, which are made in the liver and excreted into the small intestine via the gall bladder. The bile salts have a hydrophobic and a hydrophilic side and can thus surround the fat. The hydrophilic side towards the water and in contact with the intestinal environment.
If the fat droplet is thus more water-soluble, the lipases can then join in, which take care of the breakdown of triglycerides into monoglycerides and free fatty acids. The broken down lipids form micelles, which are then transported to the brusbous membrane of the intestine so that these broken down fats can be absorbed by the intestinal cells.
When the micelles come close to the burshboarder, the monoglycerides and fatty acids separate from the micelles. The monoglycerides and fatty acids then diffuse through the membrane into the small intestine.
When the monoglycerides have entered the intestinal cell they form triglycerides again. The triglycerides, together with cholesterol, form the chylomicrons. The chylomicrons are packed by the Golgi apparatus into vesicles which can be transported over the intestinal wall. These vesicles are too big to enter the capillary, so they are transported by the lymphatic system. This whole process is shown in figure 5.
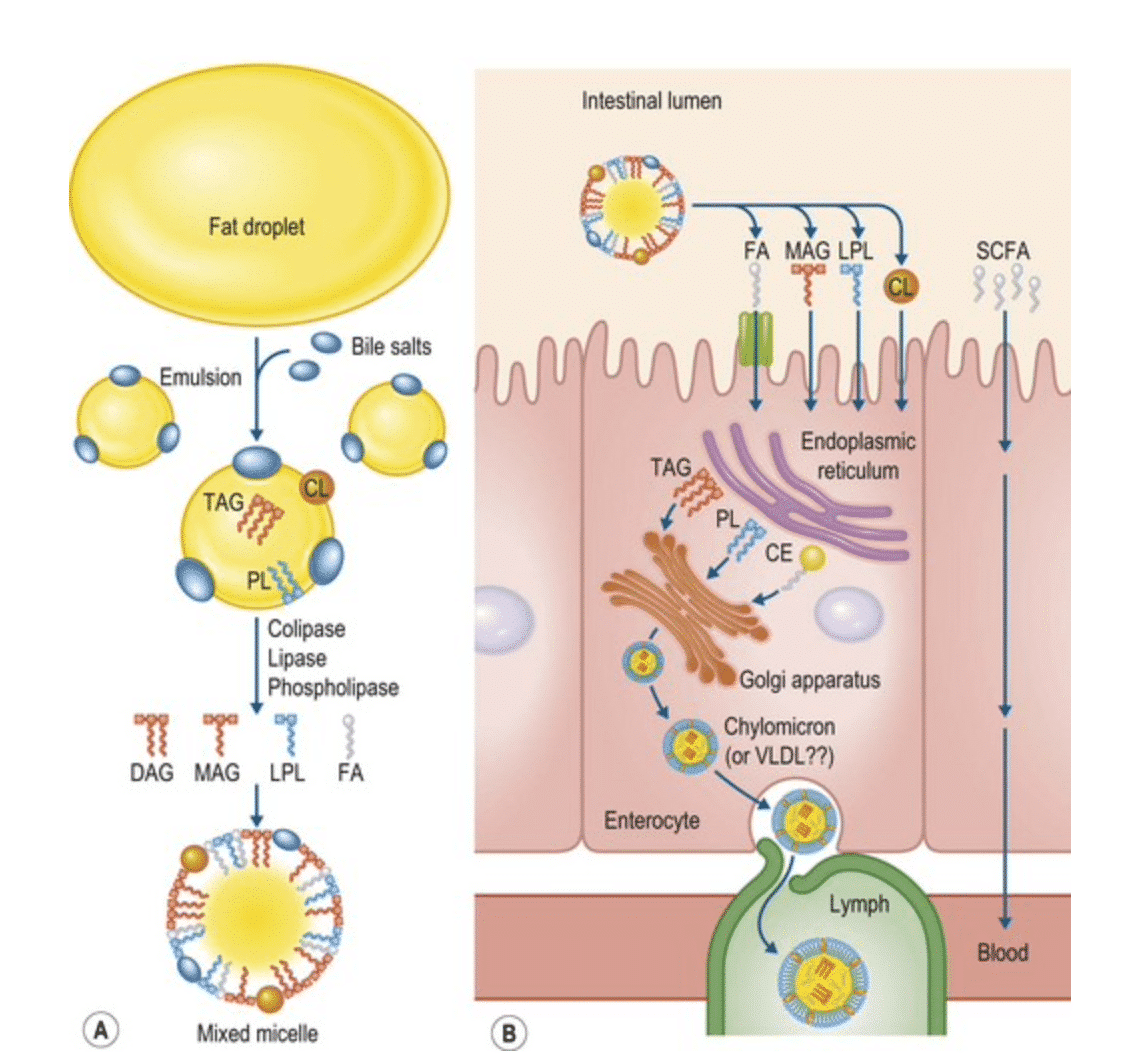
Figure 5.
Digestion of protein
Proteins are chains of amino acids, the largest kind, very long chains are called polypeptides. In order for the peptides to be absorbed properly, the peptide bonds between the amino acids must be broken. There are two different types of enzymes for breaking the bonds. Endopeptidase and exopeptidase.
The endopeptidase, which includes pepsin and trypsin, can only break polypeptides in the middle of the chain. This results in two smaller peptides. The exopeptidase cannot break a peptide bond in the middle but only at the end of the protein. This creates loose amino acids and small peptide chains. A well-known exopeptidase is carboxypeptidase, which is secreted by the pancreas.
The somewhat larger pieces, chains of 2 to 3 peptides, are co-transported with an H+ across the membrane. Now they can either be broken down by peptidase in the cell into amino acids or they can be transported to the blood with the same H+ co-transporter.
Another way of transporting slightly larger peptides is transcytosis. These are a kind of vesicles with which the molecules can be transported across the cell.
The digestive system: a summary
Digestion runs from your mouth, through your oesophagus to the stomach. There is a short pause for digestion. From there your food is transported to the small intestine and then to the large intestine. Digestion of nutrients in the small intestine is accompanied by the secretion of hormones and bile that are produced in the pancreas and the liver.
Large carbohydrates are reduced in size by the enzyme amylase to which the small molecules can be transported into the blood by a secondary active transport.
Fats are broken down into monoglycerides and free fatty acids after which, with the help of bile salts, they are water-soluble and can be packed into micelles. The micelles can enter the cell. After this, the monoglycerides and free fatty acids form triglycerides again and can be transported via the lymphatic system through the body with the help of the Golgi apparatus.
Proteins must be broken down from large peptides into small amino acids or short peptides. These can be co-transported with an H+ ion across the cell membrane, after which they are transported to the blood with the same transporter.